Introduction to Medical Coding
Unlock the Language of Healthcare: Start Your Coding Journey Now!
Dive into the heart of healthcare systems, gaining mastery in translating complex medical language into universal codes that drive effective communication across the industry. This course is more than just educational--it's transformative. You'll emerge as an indispensable asset, equipped with knowledge that skyrockets your career and enhances healthcare delivery on a global scale.
Join a thriving community of learners who have already unlocked new professional heights and personal satisfaction. Enroll now, and embrace the opportunity to shape the future of healthcare through the power of coding. This isn't just a course; it's your launchpad to becoming a pivotal player in a rapidly growing field. Commit today and make a meaningful impact tomorrow.
20 Hours average completion time
2.0 CEUs
14 Lessons
22 Exams & Assignments
132 Discussions
18 Reference Files
123 Articles
Mobile Friendly
Last Updated January 2026
In the fast-paced and ever-evolving world of healthcare, accurate communication is critical to ensuring quality patient care and efficient administrative processes. One of the most crucial, yet often overlooked, components of this system is medical coding. Medical coding acts as the bridge between clinical care and the administrative world, enabling healthcare providers, insurance companies, and government agencies to communicate seamlessly and accurately. Our Introduction to Medical Coding course is designed to equip you with the knowledge and skills necessary to become proficient in this essential field, transforming you into a vital player in the healthcare industry.
This self-paced, online course allows you to learn at your own convenience, making it perfect for busy professionals, students, or anyone looking to enter the healthcare field. With more than 6,000 students already enrolled and benefiting from the course, this program has proven to be highly effective and accessible. The average course rating of 4.28 stars speaks to its quality and relevance, helping individuals achieve real-world skills that are in demand in today's healthcare environment.
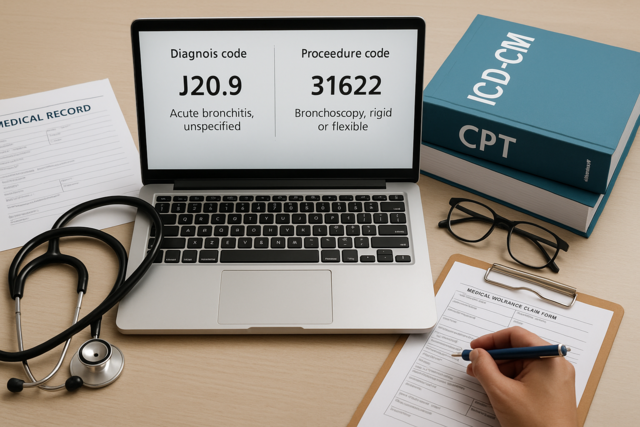
The core of medical coding lies in translating complex medical diagnoses and procedures into universal codes. These codes not only standardize communication across the healthcare industry but also play a vital role in the reimbursement process, ensuring that healthcare providers are compensated for their services. By mastering medical coding, you are not just learning a skill-you're becoming an essential link in the healthcare chain, helping ensure patients receive proper care, providers are accurately reimbursed, and medical records are efficiently managed.
Medical coding requires meticulous attention to detail and a deep understanding of medical terminology, anatomy, and healthcare procedures. Our course is designed to guide you through this intricate subject matter in an engaging and approachable way. Whether you are a newcomer with no prior experience or a seasoned professional looking to refresh your skills, this course provides you with all the tools you need to succeed.
With 14 comprehensive lessons covering topics such as diagnosis coding, procedural coding (CPT), and the International Classification of Diseases (ICD-10), you will gain a solid understanding of how to code for everything from routine medical checkups to complex surgical procedures. The course also delves into specialized areas of coding, such as anesthesia and radiology, ensuring you are well-versed in a broad spectrum of medical scenarios. You'll also explore the critical ethical aspects of medical coding, with lessons addressing issues like fraud and abuse, ensuring you are not only skilled but also conscientious in your professional practice.
The flexibility of this online course means you can learn at your own pace, making it easy to fit into your busy schedule. The estimated completion time is approximately 20 hours, but you can adjust the learning experience to meet your needs. Each lesson builds on the previous one, allowing you to gradually develop your coding expertise without feeling overwhelmed.
As you progress through the course, you'll have the opportunity to apply what you've learned through interactive assignments and exams, designed to reinforce your knowledge and ensure you are well-prepared for real-world coding scenarios. By the end of the course, you'll be able to confidently navigate the medical coding landscape, from selecting the correct codes to understanding the impact they have on patient care and healthcare reimbursement.
Upon successful completion of the course, you will earn Continuing Education Units (CEUs), which are recognized by professional organizations and employers across the healthcare industry. This official certification can be displayed on your resume, shared via social media, or used to advance your career in medical coding, billing, or healthcare administration.
Medical coding is more than just a technical skill-it's a gateway to a rewarding and in-demand career in healthcare. As healthcare systems around the world continue to evolve, the need for qualified medical coders grows, with the U.S. Bureau of Labor Statistics projecting an above-average growth rate for jobs in medical records and health information management. By enrolling in this course, you are positioning yourself at the forefront of this dynamic field, gaining the expertise needed to contribute meaningfully to the healthcare ecosystem.
Join thousands of other students who have already taken this vital step toward a brighter future. By mastering medical coding, you will not only open the door to numerous career opportunities but also play a pivotal role in enhancing the quality and efficiency of healthcare systems globally. Dive into the world of medical coding today, and become an indispensable part of the healthcare team.
- Understand ethical and legal aspects of coding
- Comprehend specialized areas like anesthesia and radiology
- Promote consistency and communication in healthcare
- Translate medical diagnoses into standardized codes
- Master medical terminology and coding systems
- Prevent healthcare fraud and ensure compliance
- Ensure accurate healthcare billing and reimbursement
- Utilize CPT and ICD-10 for diverse procedures
- Enhance patient care through precise documentation
- Efficiently navigate electronic health records
-

Digital Wedding Photography 101
-

Caring for Patients with HIV/AIDS
-

Aging and Long Term Care
-

Comprehensive Medical Terminology 1 & 2
-

Second Grade Curriculum
-

Astronomy 101
-
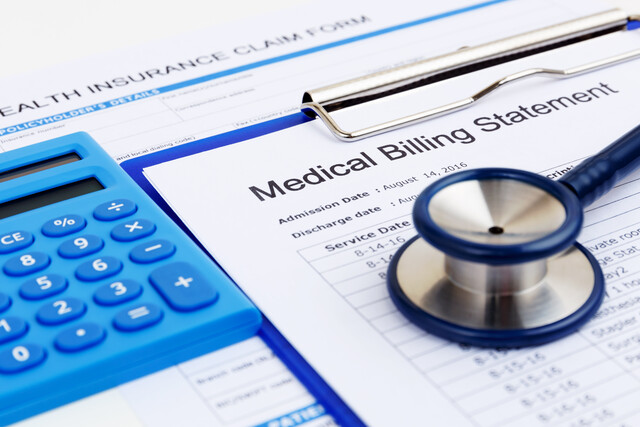
Introduction to Medical Billing
-

Marketing 101
-

Caring for Seniors
-

Business Consulting 101
-
Vegetarian Living: Discover the World Beyond Meat
-

Alzheimer's Disease 101
-

Medical Billing and Coding Course Bundle
-
Understanding Concussions
-

Microbiology Mastery: Unlocking the Foundations of Life
-

Anatomy and Physiology 101
-

CPT Coding for Beginners
-
Diabetes 101
-
Introduction to Cell and Molecular Biology
-

Problem Solving Strategies
-

HIV: Prevention, Diagnosis, Treatment
-

Medical Office Management
-

Advocacy for Elderly Patients
-
History's Greatest Conspiracies
-

HIPAA Compliance 101
