Introduction to Medical Billing
Unlock Your Future in Healthcare Administration Today!
17 Hours average completion time
1.7 CEUs
10 Lessons
10 Exams & Assignments
333 Discussions
19 Reference Files
90 Articles
Mobile Friendly
Last Updated January 2026
Mastering Medical Billing: Your Pathway to a Rewarding Healthcare Career
The healthcare industry is a vast, dynamic, and essential sector, with myriad specialties and vocations. Among these, medical billing stands out as a critical cog in the medical machinery. As the healthcare sector continues to expand, the role of a proficient medical biller becomes increasingly indispensable.
Why Medical Billing?
In our interconnected world, where patient care seamlessly merges with technological advancements, the medical biller emerges as a bridge between healthcare providers and insurance companies. They play a quintessential role in ensuring the financial health of medical establishments. From processing insurance claims to adhering to ever-evolving healthcare policies, a medical biller's responsibilities are both diverse and integral. The demand for skilled medical billers has surged in recent years. Hospitals, clinics, and private practices rely heavily on adept billers to streamline their operations and maintain fiscal health.
What Will You Learn?
This comprehensive, self-paced course is meticulously crafted to arm you with the essential skills required to excel in medical billing. It's structured to suit both novices and those looking to brush up on their skills. Designed in accessible language, this course promises a deep dive into the intricate world of medical billing.
-
Overview of the Healthcare System & Career Opportunities in Medical Billing (Lesson 1): Gain insights into the healthcare system's landscape and the exciting career paths open to medical billers.
-
Medical Biller Job Description (Lesson 2): Delve into the specifics of what a medical biller does, understanding the nuances and intricacies of the role.
-
Analyzing Provider and Patient Information (Lesson 3): Learn the art of dissecting critical data, ensuring accurate billing and top-notch patient care.
-
ICD-10-CM - What is it? (Lesson 4): Get acquainted with the International Classification of Diseases, Tenth Edition, Clinical Modification - an essential tool for medical billing.
-
Analyzing the Hospital Billing Process (Lesson 5): A deep dive into the billing process of hospitals, understanding the differences and nuances from other medical establishments.
-
Analyzing the Physician Billing Process (Lesson 6): Gain a comprehensive view of how billing works specifically for physicians, unraveling the unique challenges and solutions.
-
Exploring Different Types of Health Insurance (Lesson 7): Understand the diverse insurance types, ensuring effective communication with insurance providers.
-
Medicare Overview (Lesson 8): Discover the workings of Medicare, one of the most significant health insurance programs.
-
Reimbursement & Legal Issues (Lesson 9): Navigate the legal framework surrounding medical billing and understand the pivotal role of reimbursements.
-
Medical Billing & Coding Certifications Information (Lesson 10): Explore the various certifications available, understanding their relevance and the advantages they bring to your career.
Why Choose This Course?
For those aspiring to make a mark in the healthcare administration domain, this course serves as a beacon. You will not only learn the technical aspects of medical billing but also cultivate a holistic understanding of its role in the broader healthcare spectrum. By the course's end, you'll be poised to seamlessly integrate into any medical establishment, wielding the dual weapons of knowledge and confidence.
In conclusion, if you're seeking a career that blends the gratification of being part of the healthcare industry with the satisfaction of a meticulous administrative role, medical billing is your answer. And this course, with its extensive curriculum and practical insights, is the perfect springboard to launch you into this rewarding profession.
- Adapting to healthcare technology advancements
- Understanding medical coding and insurance protocols
- Pursuing medical billing certifications
- Navigating Medicare and government insurance programs
- Managing reimbursements and legal considerations
- Analyzing healthcare systems and billing processes
- Facilitating communication between providers and insurers
- Ensuring accuracy in claim submissions
-

Auras: Viewing, Identifying, and Understanding
-

Buddhism 101: The Principles of Awakened Living
-

Retirement Tips
-

The Art of Setting Goals
-

Elemental Magick: Harnessing Nature's Forces
-

Child Abuse Recognition, Investigation, and Protection
-
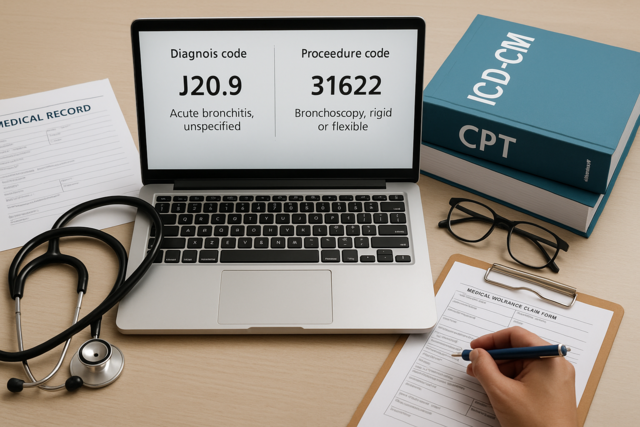
Introduction to Medical Coding
-

Anatomy and Physiology 101
-

Workplace Violence: A Guide to Responding and Preventing
-

Asthma 101
-
Human Resources Productivity Course Bundle
-

Caring for Patients with HIV/AIDS
-
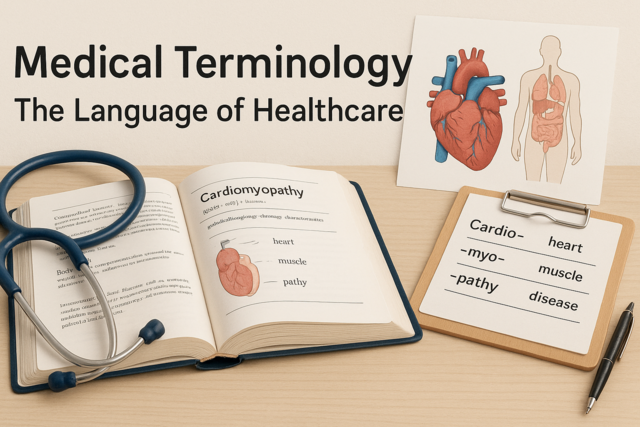
Medical Terminology 101
-

Business Management
-

Aging and Long Term Care
-

ICD-10: Medical Coding
-
Understanding Concussions
-

Business Budgeting 101: How to Plan, Save, and Manage
-

Understanding Insurance Types
-
Diabetes 101
-

How to Teach Reading Fundamentals
-

Medical Billing and Coding Course Bundle
-

Medical Terminology 201
-

Creative Writing for Beginners
-

End of Life Care